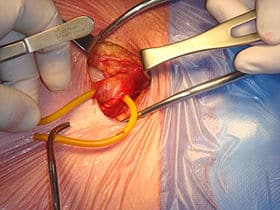
An inguinal hernia is a protrusion of the abdominal-cavity contents in the groin area. Inguinal hernia surgery is an operation that is carried out to correct the bulge due to inguinal hernia by returning displaced tissues and organs to their original position.
Hernias typically do not go on their own therefore surgery remains the ultimate treatment option. Inguinal hernia surgery is one of the most commonly performed operations in the world and it’s the most commonly performed surgery in the United States.
Inguinal hernia surgery
Indication for Inguinal Hernia Surgery
Some factors that determine whether hernia surgery is to be performed include:
– Severity of symptoms
– Type of hernia
– Surgical history
– Size
– Health of the patient
Hernia repair surgery may be performed as elective surgery, i.e. planned, in people who have symptoms that interfere with their normal level of activity and a continual increase in the size of the hernia.
The repair is performed in an emergency if there is strangulation of the tissues. Symptoms of strangulation include:
- Fever
- Nausea and vomiting
- Extreme pain in the affected area
- Difficulty if passing gas or stool.
Emergency surgical repair of the hernia is required to save the strangulated tissues.
Contraindications of Inguinal Hernia Surgery
An inguinal repair is not to be performed under certain conditions due to significant risks that may be involved. Surgery is not recommended in patients who have:
– Unstable medical conditions
– Active infection within the groin or bloodstream
– Pregnancy
Laparoscopic surgical technique is not suitable for patients with:
– Previous radiation therapy to the pelvis
– Prior major open abdominal
– Complex Hernia
– Inability to undergo general anesthesia
Surgical Techniques
The first differentiating factor in hernia repair is whether the surgery is done openly, or laparoscopically.
The surgical approach employed depends on factors such as features of the hernia, the person’s anesthetic needs, and the surgeon’s experience with either technique.
Open Hernia Repair
Open hernia repair is when an incision is made in the skin directly over the hernia. All techniques involve an approximate 10-cm incision in the groin. Once exposed, the hernia sac is returned to the abdominal cavity or excised and the abdominal wall is reinforced with mesh or the patient’s own tissues.
Open repairs are classified into; Open mesh repairs and Open tension repair depending on whether a mesh or patient’s own tissues are utilized to repair the weakness.
Mesh repairs enable surgeons to repair hernias without causing undue tension in the surrounding tissues while reinforcing the abdominal wall. Repairs utilizing the patient’s own tissue to repair the weakness have been shown to cause undue tension and increase the likelihood of the hernia recurring.
One large benefit of open hernia repair lies in its ability to tailor the anesthesia to a person’s needs. People can be administered local anesthesia, a spinal block, as well as general anesthesia.
Laparoscopic repair
Laparoscopic hernia repair is when minimally invasive cameras and equipment are used and the hernia is repaired with only small incisions adjacent to the hernia.
There are two main methods of laparoscopic repair: transabdominal preperitoneal (TAPP) and extra-peritoneal (TEP) repair.
Laparoscopic repair uses mesh for reinforcement, so it has a lower recurrence rate. Plus, a smaller incision means less discomfort after surgery, little to no scarring, and a quicker return to normal activity. Many people return to work within a few days.
While open hernia repair may be done under general, regional (spinal), or even local anesthesia with sedation, laparoscopic hernia repair is always done under general anesthesia.
Complications of Inguinal Hernia Surgery
Like all surgical procedures, there are risks involved. These include:
– bleeding
– Infection
– Fluid collection
– Damage to surrounding structures such as nerves, blood vessels, or the bladder
Risks specific to inguinal hernia surgery include:
– Recurrence of hernia
– Impairment of sexual activity
– In males, injury to the scrotum, vas deferens and other organs
Inguinal Hernia Surgery Cost
The cost of inguinal hernia surgery depends on several factors such as the location of the hospital, the surgical approach and health insurance plan.
A recent study of more than 1.5 million hernia operations found that the average cost for an open hernia surgery ranged between $4,200 and $6,200.
Those with insurance can expect to pay typical deductibles and coinsurance rates. According to the Medical Expenditure Panel Survey conducted by the Agency for Healthcare Research and Quality, the average family will have a $939 deductible to meet each year before their insurance benefits cover procedures.
In addition, the survey found that the average coinsurance rate is about 17.9 percent of the bill. This means the average patient would pay between $750 and $1,109 for their hernia surgery.
Recovery from Inguinal Hernia Surgery
Upon awakening from anesthesia, patients are monitored for their ability to drink fluids, produce urine, as well as their ability to walk after surgery. Most patients are then able to return home once those conditions are met. It is common for patients to experience residual soreness for a couple of days after surgery.
Patients are encouraged to make strong efforts in getting up and walking around the day after surgery. Most patients can resume their normal routine of daily living within the week such as driving, showering, light lifting, as well as sexual activity. Long work absences are rarely necessary and the length of sick days tend to be dictated by respective employment policies.
In general, it is not recommended to administer antibiotics as prophylaxis after elective inguinal hernia repair. However, the rate of wound infection determines the appropriate use of the antibiotics
You should contact your doctor immediately if you notice the following symptoms:
- fever greater than 39C/101F
- progressive swelling of the surgical site
- severe pain
- recurring nausea or vomiting
- worsening redness around incisions
- drainage of pus from incisions
- difficulty or lack of producing urine
- new-onset shortness of breath