Sleep apnea is a sleep disorder in which there is intermittent stoppage of breathing during sleep. Each pause can last for a few seconds to a few minutes and they happen many times a night.
As a result of this, the person with sleep apnea usually feels sleepy or tired during the day.
Sleep apnea can be divided into two main forms depending on the cause:
1. Obstructive sleep apnea (OSA) – This is the more common form and is caused by a blockage of the airway, usually when the soft tissue in the back of the throat collapses during sleep.
2. Central sleep apnea (CSA) – CSA is due to the failure of the brain to signal the muscles to breathe, due to instability in the respiratory control center.
Risk factors for the development of sleep apnea
Sleep apnea can affect people regardless of sex, race, or age. However, risk factors include:
- being male
- obesity
- age over 40
- large neck circumference (greater than 16–17 inches)
- enlarged tonsils or tongue
- small jaw bone
- gastroesophageal reflux
- allergies
- sinus problems
- a family history of sleep apnea
- deviated septum
Alcohol, sedatives, and tranquilizers may also promote sleep apnea by relaxing throat muscles. People who smoke tobacco have sleep apnea at three times the rate of people who have never done so.
Central sleep apnea is more often associated with any of the following risk factors:
- being male
- age above 65
- having heart disorders such as atrial fibrillation or atrial septal defects such as PFO
- stroke
High blood pressure is very common in people with sleep apnea.
Sleep Apnea Treatment
Sleep apnea can be treated via several means including lifestyle changes, breathing devices and surgery. Sleep apnea surgery is often reserved as a third line of treatment when medications and breathing devices are ineffective.
Lifestyle Changes
First of all, patients are told to avoid substances that can relax throat muscles causing the collapse of the airway at night. These lifestyle changes include:
- Avoidance of alcohol
- Quit smoking
- Stop taking sleeping pills
Another lifestyle change to treat sleep apnea is weight loss. Excess body weight is thought to be an important cause of sleep apnea.
People who are overweight have more tissues in the back of their throat which can restrict the airway especially when sleeping.
In weight loss studies of overweight individuals, those who lose weight show reduced apnea frequencies and improved Apnoea–Hypopnoea Index (AHI)
Breathing Devices

For moderate to severe sleep apnea, the most common treatment is the use of a continuous positive airway pressure (CPAP) or automatic positive airway pressure (APAP) device. This splints the person’s airway open during sleep using pressurized air.
The person typically wears a plastic facial mask, which is connected by a flexible tube to a small bedside CPAP machine.
Although CPAP therapy is effective in reducing apneas and less expensive than other treatments, some people find it uncomfortable.
Some complaints of feeling trapped, having chest discomfort, and skin or nose irritation. Other side effects may include dry mouth, dry nose, nosebleeds, sore lips and gums
Sleep Apnea Surgery
Surgery is often is resorted to when other treatment methods are rejected or ineffective. Surgical treatment for obstructive sleep apnea needs to be individualized to address all anatomical areas of obstruction.
There are many different types of surgery for sleep apnea and snoring and they include:
1. Adenoidectomy and tonsillectomy
Children with obstructive sleep apnea typically have enlarged tonsils and adenoid tissue. Surgery on children is over 80% successful by simply performing an adenoidectomy and tonsillectomy.
Some adults with large tonsils may be candidates for having their tonsils and/or adenoids removed either alone or in combination with other procedures, such as uvulopalatopharyngoplasty (UPPP) or nasal surgery.
2. Uvulopalatopharyngoplasty (UPPP)
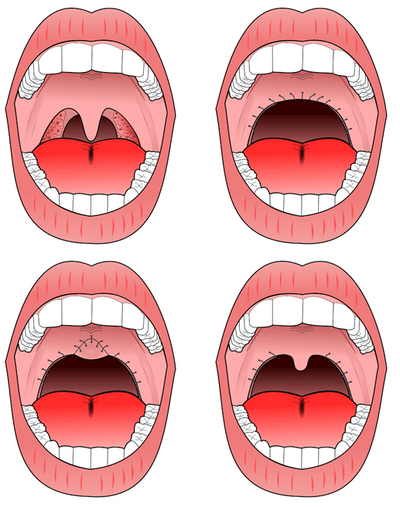
Uvulopalatopharyngoplasty. A) pre-operative, B) original UPPP, C) modified UPPP, and D) minimal UPPP.
The procedure most commonly performed for sleep apnea is the uvulopalatopharyngoplasty (UPPP).
This involves removal of the tonsils if still present, and a subsequent palatal procedure. The tonsil pillars are often sutured closed—and the uvula is either trimmed, cut, folded, reshaped, or sutured to the soft palate.
3. Hyoid suspension
Hyoid suspension, also known as hyoid myotomy and suspension or hyoid advancement, is a surgical procedure or sleep surgery in which the hyoid bone and its muscle attachments to the tongue and airway are pulled forward to increase airway size and improve airway stability in the retrolingual and hypopharyngeal airway (airway behind and below the base of tongue).
4. Genioglossus Advancement
During sleep, the tongue can fall back to block the space for breathing in your throat. This type of sleep apnea surgery moves the major tongue attachment forward, opening up space for breathing behind the tongue.
It involves making a cut in the lower jaw where the tongue attaches. This piece of bone (but not the entire jaw) is then moved forward.
5. Maxillomandibular osteotomy (MMO) and advancement (MMA)
This type of surgery is a treatment option for severe sleep apnea. It moves your upper and/or lower jaw forward to enlarge the space for breathing in the entire throat.
The procedures involve cutting the bone of your jaws, which then heal over the course of months. Your jaws may be wired shut for a few days. Your diet also will be limited for several weeks after the procedure.
Related: Le Fort Osteotomies
6. Tracheostomy
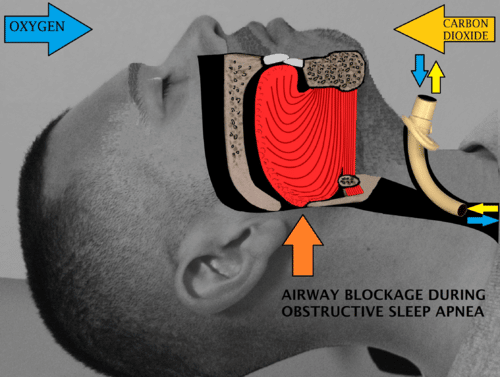
Tracheostomy, bypassing the area of airway obstruction during sleep.
This surgery is an effective treatment for sleep apnea. But it is a drastic option that is used in rare, emergencies. Other treatment options are preferable for almost all patients with sleep apnea. It involves placing a hollow breathing tube directly into your windpipe in the lower portion of the neck.
This tube can be plugged in during the day, allowing you to breathe and speak normally through your nose and mouth. At night the tube is opened to allow you to breathe without any blockage in your throat.
7. Weight loss surgery
Bariatric surgery can promote weight loss and may improve sleep apnea in people who are obese. But weight loss surgery usually is recommended because of other health risks related to obesity.
Prior to weight loss surgery, you may be referred to a sleep physician for an evaluation and sleep study. There are many types of weight loss surgery. Some procedures reduce the size of the stomach, making it harder to eat as much food.
Each surgery has different risks and benefits. People who are obese should work with their doctor to implement other weight loss strategies before considering surgery. You should use CPAP before and after weight loss surgery.
Risks and Complications
Every surgical procedure usually carries with it the risk of complications. Some complications with the sleep surgeries include bleeding, infection, swelling, sore throat, etc.
Patients are advised to consult with their doctors in case of severe complications that don’t resolve on their own.
More: Jaw Reduction Surgery


